[This information guide is also available in PDF format to download.]
Introduction
Breast cancer is common, affecting 1 in 8 Australian women by the age of 85. More than 90-95% of breast cancers occur in women who do not have a strong family history of breast cancer. In the other 5-10% of individuals who develop breast cancer, there will be an underlying heritable gene fault (sometimes referred to as a pathogenic variant) that has contributed to the cancer diagnosis. These gene faults can be passed through men and women in families, from one generation to the next. Any female family member who inherits this gene fault is at an increased risk of developing breast cancer. The same gene faults that increase the risk of breast cancer can also increase the risk of cancer of the ovaries and fallopian tubes.
This brochure contains information for women who have been assessed by a family cancer clinic as being at high risk of developing breast cancer and cancer of the ovaries and fallopian tubes, including:
- women who have had genetic testingand been found to carry a fault in a highrisk breast and ovarian cancer gene(such as BRCA1, BRCA2 or PALB2).
- women who have been assessed ashaving a potentially high risk ofdeveloping breast and/or ovarian/fallopian tube cancer – this could be dueto their family history (sometimes incombination with other risk factors).
This brochure explains the options for managing breast and ovarian/fallopian tube cancer risk, including strategies to detect a cancer early, or in some cases, significantly reduce the risk of cancer developing.
Am I at high risk?
Less than 1% of the Australian population is at high risk of developing breast cancer and cancer of the ovaries and fallopian tubes.
Women who may be at high risk of these cancers have:
- had genetic testing and been found to carry a fault in a high-risk breast/ ovarian cancer-associated gene (such as BRCA1, BRCA2 or PALB2).
- a very strong family history of breast and ovarian cancer.
In addition to BRAC1, BRAC2 and PALB2, there are other genes in which faults can also increase the risk of cancer. However, finding faults in these genes is even more rare.
How high is my risk?
The lifetime risk of breast cancer and cancer of the ovaries and fallopian tubes varies depending on the type of gene fault in your family.
For women with a BRCA1 gene fault
- the lifetime risk of breast cancer is between 65% and 79%
- the lifetime risk of ovarian and fallopian tube cancer is between 36% and 53%
For women with a BRCA2 gene fault
- the lifetime risk of breast cancer is between 61% and 77%
- the lifetime risk of ovarian and fallopian tube cancer is between 11% and 25%
For women with a PALB2 gene fault
- the lifetime risk of breast cancer is between 44% and 63%
- the lifetime risk of ovarian and fallopian tube cancer is between 2% and 10%
An individual’s risk of developing these cancers is influenced by other factors, such as their family history, lifestyle factors, breast density and other genetic risks (such as polygenic scores). These factors can be incorporated using modelling to to provide a personalised risk assessment for women with faults in a breast/ovarian cancer-associated gene. People who carry these gene faults may also be at increased risk of other cancers. These are discussed later in this brochure.
About breast cancer
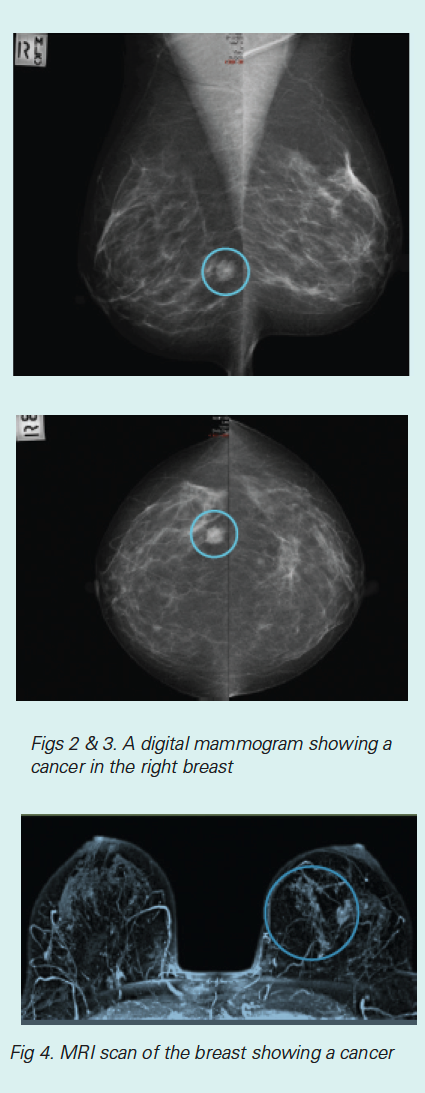
Breast cancer is very common, so a family history of breast cancer is also quite common. Most women who develop breast cancer do not have an inherited gene fault. In many cases, breast cancer can be found early using screening mammograms (or other imaging tests such as breast ultrasound or magnetic resonance imaging (MRI).
These tests may find a cancer before a woman can feel a lump in her breast. Even when breast cancer is found when a lump can be felt, there is a very good outlook. Modern treatments for breast cancer include surgery to remove the affected part of the breast (wide local excision or lumpectomy followed by radiotherapy) or the whole breast (mastectomy). This is often followed by chemotherapy and/or targeted therapy.
Women who carry a BRAC1, BRAC2 or PALB2 gene fault tend to develop breast cancer in both breasts over time. The breast cancer that develops in these women is similar to breast cancer in other women, though there is an over-representation of the triple negative type of cancer in BRAC1 and BRAC2 gene fault carriers. When breast cancer is found early, women who carry these gene faults seem to have a similar survival rate to other women with breast cancer. Further research is underway to clarify this.
About ovarian cancer
Cancer of the ovaries and fallopian tubes is much less common than breast cancer. It affects 1 in 100 women in the general population, so a family history of ovarian cancer is less common.
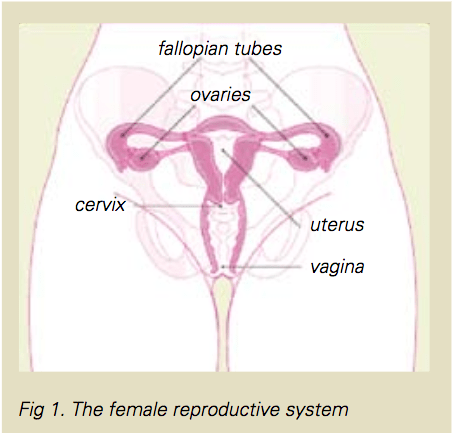
Women who carry a BRCA1, BRCA2 or PALB2 gene fault have an increased risk of cancer of the ovaries and fallopian tubes. The ovaries are the organs in the female pelvis that produce eggs and produce the hormones oestrogen and progesterone.
The ovaries release an egg each month (ovulation) in the years before menopause.
Pap smears and cervical screening tests do not test for or pick up cancer of the ovaries or fallopian tubes. These screen for cancer of the cervix (the opening of the uterus or womb).
The symptoms of ovarian cancer and cancer of the fallopian tubes are vague, and can be caused by lots of things other than ovarian cancer. Symptoms which may indicate ovarian cancer if they are continuous or persistent (lasting weeks or months) include:
- a swollen abdomen (tummy)
- pain or pressure in the abdomen
- a feeling of bloating and fullness
- vaginal bleeding different to your normal monthly period
- urinary changes (urgency or frequency)
- bowel changes (diarrhoea, constipation or flatulence)
- nausea or indigestion
- gaining weight or losing weight
- feeling tired
- pain in the lower back
Because the symptoms are so vague, this type of cancer is difficult to diagnose. It is often not found until it is quite advanced. Survival from ovarian cancer depends on its stage when it is found.
Treatment for ovarian cancer and cancer of the fallopian tubes varies depending on its stage. Treatment often includes surgery, chemotherapy and sometimes targeted therapy (and radiotherapy, but this is rare). It is uncommon for advanced ovarian cancer to be cured.
Screening for cancer of the ovaries and fallopian tubes
Women at high risk of ovarian and fallopian tube cancer are advised to consider surgery to reduce their risk (see next section). Screening for ovarian cancer is difficult. Unlike breast cancer, which can be detected early with breast imaging, there are no screening tests that reliably pick up ovarian cancer at an early stage. Screening with transvaginal ultrasound of the ovaries and measuring CA125 levels in the blood is not recommended. Evidence from large research trials shows that these tests do not effectively pick up ovarian cancer early.
What tests can I have to screen for breast cancer?
Screening for breast cancer is well established. Screening tests aim to pick up cancer before it causes symptoms. It is known that survival from breast cancer is highest when it is picked up at this early stage. Screening tests for breast cancer may include:
- Breast MRI; this is used to screen women under the age of 60 at high risk of breast cancer. Research has shown that MRI can pick up breast cancer at an earlier stage. Breast MRI, in addition to finding cancer early, has a high ‘false positive’ rate. This means that it also picks up changes that are not cancerous, which may lead to unnecessary worry and biopsy.
- Mammograms; these have been proven to find breast cancer at an early stage and to improve survival in the general population. This has not yet been proven in young, high-risk women. Digital breast tomosynthesis, also known as 3D mammography, is an advanced form of breast mammography that takes multiple images of the breast from different angles and then reconstructs these into a 3D image. This may be beneficial in women with more dense breast tissue.
- Breast ultrasound; this is sometimes used as a screening test but is most useful as an additional test when there is concern after a clinical examination, MRI or mammogram. It has not been proven to be a reliable screening test for breast cancer by itself.
- Checking your own breasts for lumps and visiting your doctor each year for a breast examination are other ways to find breast cancer, although these checks do not always lead to an earlier diagnosis and improved survival. It is also important to seek timely medical review in the event that there are new breast changes.
What can be done to reduce my risk?
There are several things that can lower your risk of developing breast cancer and cancer of the ovaries and fallopian tubes. The risk can never be reduced to zero, but it can be reduced to a level equal to or even lower than that of the average woman who does not carry a gene fault.
Things that can reduce the risk of breast cancer are:
- surgery to remove the breasts
- medication that may reduce the risk of breast cancer
Things that can reduce the risk of cancer of the ovaries and fallopian tubes are:
- surgical removal of the ovaries and fallopian tubes
- use of the oral contraceptive pill
These ways of reducing the risk of cancer will not interest everyone who is at high risk. These are very personal decisions. Being aware of the options may make it easier to know what is right for you.
The emotional aspects of risk-reducing surgery
Every women reacts differently to the idea of risk-reducing surgery. It is a big decision to have your breasts and/or your ovaries and fallopian tubes removed to reduce the risk of cancer.
Some women who carry a gene fault have seen lots of women in the family die of breast or ovarian cancer and feel they would like to do whatever they can to minimise their own risk.
Others feel that the thought of losing their breasts is worse than the thought of developing cancer. These women may prefer to take medication to reduce the risk of cancer or to have close monitoring.
Some women find a combination of both approaches suitable, for example having surgery to remove their ovaries and fallopian tubes, but close monitoring (without surgery) of their breasts.
All of these approaches are perfectly reasonable. It is important that you make a decision you feel comfortable with.
Remember, you can take all the time you need to get information and consider the choices available to you. You may reconsider and have the surgery in a few years if it doesn’t feel right for you now. Many women find a consultation with a Clinical Psychologist helpful when thinking about these decisions.
Surgery to remove the breasts
Surgery to remove the breasts dramatically reduces the risk of breast cancer (by about 95%). It is impossible for a surgeon to remove every breast tissue cell, so there is still a possibility of developing breast cancer, but the risk is extremely small.
Bilateral mastectomy
Bilateral mastectomy is the operation to surgically remove both breasts. This can be done to reduce the risk of breast cancer. It is the same operation that a surgeon would perform to treat a woman who has breast cancer, except that usually the lymph nodes in the armpit are not removed. Often, the nipples can be kept when a risk-reducing bilateral mastectomy is done and this helps to make a reconstruction look more natural. There are also situations where the nipples cannot be kept, such as women with larger breasts or women who smoke. A nipple-sparing mastectomy is a safe operation to reduce the risk of cancer because all of the breast tissue underneath the skin of the nipple is removed. Breast reconstruction can be offered to nearly all women who have a mastectomy.
Choices after risk-reducing mastectomy
After a mastectomy some women choose to wear an artificial prosthesis in their bra. These prostheses are available in a range of sizes and shapes. Other women choose to have a surgical breast reconstruction. More information about surgical breast reconstruction can be found at the end of this brochure.
Surgery to remove the ovaries and fallopian tubes
Surgery to remove the ovaries and fallopian tubes (risk-reducing salpingo-oophorectomy) reduces the risk of cancer of the ovaries and fallopian tubes by up to 95%.Surgery to remove these organs is only done when you have finished having a family. It is not possible to have children after this surgery. The timing of surgery differs depending on the type of gene fault in your family and also on your own personal and family history.
-
In families that carry a BRCA1 gene fault, cancer of the ovaries and fallopian tubes usually develops after the age of40.Surgery is therefore recommended after the age of 35 and by the age of 40.
-
In families that carry a BRCA2 gene fault, cancer of the ovaries and fallopian tubes usually develops at a later age.Surgery is therefore recommendedafter the age of 40 and by the age of 45.
For women who have not completed their families, and are at the age where they have been recommended to undergo risk-reducing salpingooophorectomy, assisted reproductive organs may be an option.
Surgery to remove the ovaries and fallopian tubes can often be done by laparoscopic (keyhole) surgery which allows the operation to be done through a few tiny cuts in the tummy. The recovery from this surgery is usually quick, taking less than a week.
If you have had previous abdominal surgery, the operation may be done through a larger cut in the bikini line area.
If you are considering having surgery to remove the ovaries and fallopian tubes, your surgeon will be able to discuss these details with you. This surgery is very specialised and it is important that it is done by a surgeon who is experienced in cancer treatment and prevention.
Managing menopause after surgery
The main disadvantage of surgery to remove the ovaries and fallopian tubes before menopause is that it causes a ‘surgical menopause’. This means that you may experience all of the symptoms that a woman experiences with a natural menopause. The symptoms may be severe, as the surgery causes a sudden menopause rather than a natural menopause happening over months or years. Women who have surgery to remove their ovaries after they have their natural menopause (and have some menopausal symptoms) should not feel their symptoms any more intensely after their surgery.Some of the symptoms of menopause that you may experience after having the ovaries removed include:
- hot flushes
- mood swings
- vaginal dryness
- painful intercourse
- reduced libido or sexual desire
- urinary symptoms and infections
- osteoporosis (thinning of the bones and bone fractures)
The severity of these symptoms is very individual and is difficult to predict. Menopausal symptoms may diminish with time, but in some women may be present for many years. There are, however, lots of treatments available to control these symptoms and to lessen the effect they have on your life. Treatments for menopausal symptoms include:
- hormone replacement therapy (see next section)
- symptomatic treatments, such as vaginal moisturisers and lubricants to reduce vaginal symptoms
- antidepressant medication such as venlafaxine (Efexor) to reduce hot flushes
- ‘natural therapies’ (such as black cohosh) which may be effective for some women.
The choice of treatment will depend on many factors and may be different for those who have already had a diagnosis of breast cancer.
Hormone replacement therapy
Hormone replacement therapy (HRT) usually refers to the use of hormones by women after menopause. HRT can be used in the form of vaginal medication, skin patches, implants or tablets. The usual hormones used in HRT are:
- oestrogen alone (only used in women who have had a hysterectomy)
- oestrogen and a progestogen in combination
Some people worry about taking HRT because there has been some research showing that HRT after the menopause can cause a small increase in the risk of breast cancer. More recent research, however, has shown that HRT is safer than once thought.
If HRT is used for less than five years, around the time of natural menopause (around age 50), the risk of breast cancer related to HRT is very low.
In women who carry a gene fault increasing the risk of breast cancer, HRT may be used to treat severe symptoms of menopause after surgery to remove the ovaries and fallopian tubes.
This surgery is often done when a woman is aged 35 to 45, many years before she would have had a natural menopause.
HRT should generally be avoided in women who have had breast cancer in the past.
Medication to reduce the risk of breast cancer
There are some medications that have been proven to reduce the risk of breast cancer in women who are at higher risk. It is not known whether a similar lowering of risk occurs in women with a BRCA1 or BRCA2 gene mutation.
Tamoxifen is often used to treat breast cancer, but it may also play a role in breast cancer prevention. A five-year course of tamoxifen tablets can reduce the risk of developing breast cancer by half.
However, tamoxifen can have some rare serious side effects, such as causing blood clots in the legs or lungs, and cancer of the lining of the womb (endometrial cancer), particularly when taken after one goes through menopause.
Raloxifene is a similar medication to tamoxifen and it is approved for breast cancer risk reduction in post-menopausal women. Raloxifene can reduce the risk of breast cancer by around 60% and it has the advantage of also reducing the risk of osteoporosis.
Your doctor can talk to you about whether medication to reduce the risk of breast cancer is suitable for you. The possible risks need to be balanced against the likely benefits.
Lifestyle factors affecting your risk
There are some lifestyle and environmental factors that can alter your risk of breast cancer and ovarian cancer.
Alcohol
Even moderate alcohol consumption has been shown to increase the risk of breast cancer. There is some research showing that this also applies in high-risk women. This is one of the lifestyle changes that women can choose to make in order to reduce their risk of breast cancer. If you choose to drink, it is recommended that you limit your intake to one standard drink a day.
Reproductive factors
Having babies, particularly under the age of 30, slightly reduces the risk of breast cancer in the general population. The effect in women at higher risk is uncertain because results of research have not been consistent.
Breast feeding
Breast feeding reduces the risk of breast cancer in the general population and in women who carry a gene fault.
Oral contraceptives
These reduce the risk of ovarian cancer in the general population and in gene mutation carriers. Their effect on breast cancer r is uncertain because results of research have not been consistent. Some studies show an increase in risk and some show no effect.
Weight
Keeping your weight in the healthy range (using diet and exercise) is something practical you can do to reduce your risk of breast cancer. It can also reduce the risk of other medical problems like heart disease and diabetes. More information can be found in the Nutrition and Breast Cancer Risk brochure.
Smoking
If you are a smoker, quitting is the best thing you can do to look after your health. There are many health benefits to being a non-smoker. Women who smoke have a much higher risk of complications with surgery, especially breast surgery, and being a smoker can limit your options for breast reconstruction. You can get help with giving up smoking by speaking to your health care professionals or calling the Quitline on 13 78 48.
What happens when breast cancer develops in a woman who carries a gene fault?
If breast cancer develops in a woman who carries a gene fault, the treatment choices are mostly the same as they are for any woman.
Treatment may include mastectomy or breast conservation surgery. Radiotherapy, chemotherapy and/or hormone receptor-targeted or HER2-targeted therapy may also be recommended. In certain circumstances, women who develop breast cancer in the context of a BRCA1 or BCRA2 gene fault may also be able to access specific treatment that targets this gene fault.
Your treatment team may be more likely to recommend a mastectomy or may even recommend removing both breasts (bilateral mastectomy) if you carry a gene fault. This is because your risk of developing a breast cancer in the other breast in the future is higher than it is for other women.
The treatment for breast cancer depends on lots of factors and these will be discussed in detail with you if this situation develops.
What about other cancers?
The gene faults that increase the risk of breast cancer and cancer of the ovaries and fallopian tubes in women may also increase the risk of other cancers.
-
Faults in BRCA1 may be associated with a slightly increased risk of uterine cancer in women and a slightly increased risk of prostate cancer in men.
-
Faults in BRCA2 are associated with a slightly increased risk of male breast cancer, prostate cancer and sometimes cancer of the pancreas.
-
Faults in the PALB2 gene may be associated with a slightly increased risk of male breast cancer, prostate cancer and pancreatic cancer.
-
Li-Fraumeni syndrome is not usually associated with cancer of the ovaries and fallopian tubes, but is associated with bone, soft tissue, brain, lung or adrenal gland cancers, or leukaemia.
-
Hereditary non-polyposis colorectal cancer (HNPCC, or Lynch syndrome) is due to faults in mismatch repair genes. It is not associated with breast cancer, but is associated with bowel and other gastrointestinal, uterine and ovarian cancers.
The doctors at your familial cancer clinic will be able to discuss these issues with you in more detail.
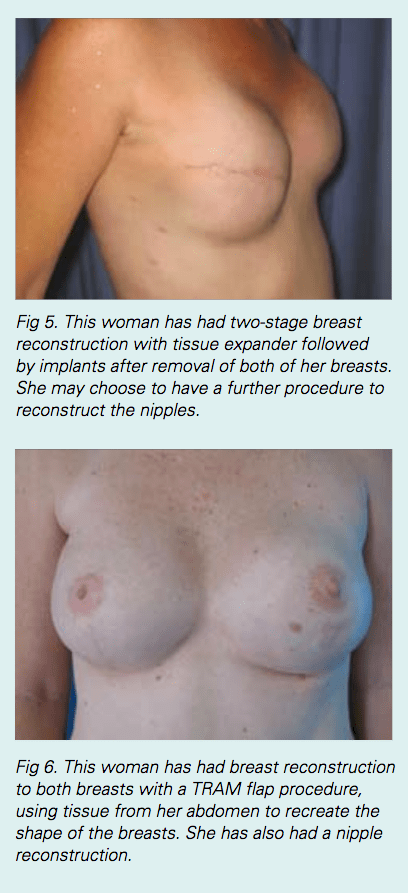
Breast reconstruction
Breast reconstruction is an option for almost every woman following risk-reducing surgery to remove the breasts. A good cosmetic result can usually be achieved with breast reconstruction to create two breasts that are similar. Breast reconstruction will never create completely normal breasts but it can give your body a shape that will look natural when you are wearing clothes.
Breast reconstruction can be done at the same time as the mastectomy (immediate reconstruction), the most common choice, or as a separate operation at a later time (delayed reconstruction).
Breast reconstruction after mastectomy can be done in two ways: using a breast implant or using natural body tissues.
There are lots of things that may influence your choice of breast reconstruction.
Your body shape, your level of physical activity, your general fitness and personal preference are all things to be considered. The costs of all types of breast reconstruction may be partly covered by private health funds.
Breast reconstruction is not for everyone, and many women choose to wear an artificial breast form (external prosthesis) in their bra rather than have surgical reconstruction.
If you are thinking about breast reconstruction, your doctor can refer you to a plastic surgeon experienced in breast reconstruction to discuss your options in detail.
More information can also be found in the breast reconstruction brochure.
How is a breast reconstructed?
There are several different surgical techniques that can be used to create a breast shape on the chest (and to match it to the opposite breast). These include:
- Breast implant reconstruction: insertion of a silicon gel implant, or insertion of a tissue expander that is replaced later with a permanent silicone gel breast implant.
- Tissue flap reconstruction: moving the tissue from the back, tummy or thigh to the chest area.
- Reconstruction of the nipple: this usually happens at a later stage, typically 3 to 12months after the implant or tissue reconstruction.
- Surgery to the unaffected breast so that it matches the reconstructed side better:”symmetrising” surgery.
Breast reconstruction using a breast implant
Breast reconstruction using a breast implant can be done in one operation or as two operations. When it is done in one operation, a permanent breast implant is used and this is usually wrapped in a mesh to give it support. There are times when a surgeon will recommend doing the operation in two stages. The first stage inserts a tissue expander, which is a device similar to an empty balloon. This is inflated (‘expanded’)
Breast reconstruction using your natural body tissue
Breast reconstruction can also be done using tissue from another part of the body to create a breast. This is usually done with tissue from:
- the lower tummy (abdomen), called a transverse rectus abdominis myocutaneous (TRAM) flap, or deep inferior epigastric artery perforator(DIEP) flap; or
- the back and shoulder blade area, called a latissimus dorsi (LD) flap, with or without an implant.
Breast reconstruction using natural body tissue is a much bigger operation than breast reconstruction using an implant. It takes many hours to perform. The recovery time is longer because there are other wounds that need to heal (the ‘donor site’ on the abdomen or back).
Useful contacts/websites
| Cancer Australia | canceraustralia.gov.au |
| Cancer Council | cancer.org.au |
| Cancer Council Helpline | 13 11 20 |
| Breast Cancer Network Australia (BCNA) | 1800 500 258 bcna.org.au |
[This information guide is also available in PDF format to download.]
Version 6 – SWP 443 March 2025
© Westmead Breast Cancer Institute 2025
