[This information guide is also available in PDF format to download.]
What is lymphoedema?
Lymphoedema is swelling that develops when lymph fluid builds up in the body’s soft tissues and does not go away. It may develop in the arm or breast/chest region after treatment for breast cancer when the lymph nodes (lymph ‘glands’) in the armpit are removed with surgery or treated with radiotherapy. Treatment to these lymph nodes can interfere with the way fluid moves through the lymphatic system, and can cause a build-up of fluid in the arm and chest. This build-up of fluid is called lymphoedema.
Lymphoedema is most common in the first eighteen months after treatment but may develop any time, including years later. Lymphoedema usually develops gradually. If you develop lymphoedema this does not mean that your breast cancer is coming back.
Most people who have treatment to the lymph nodes, however, will never develop lymphoedema. It is our goal to prevent lymphoedema occurring or at least detect it early to avoid long term problems. Prevention and early detection are the keys to success and there are things that can be done to help reduce the risk!
This brochure explains what lymphoedema is and gives you some simple guidelines to care for your arm. There are three sections:
- General information about lymphoedema.
- Guidelines for reducing the risk of lymphoedema and its impact on your everyday life.
- Information about treatment for lymphoedema.
What is the risk of developing lymphoedema?
Anyone who has treatment to the lymph nodes as part of breast cancer treatment may develop lymphoedema.
The risk is highest for people who have most of the lymph nodes removed from the axilla which is known as an axillary lymph node dissection (ALND) (up to 20%) and for those who have both ALND and radiotherapy to the lymph nodes in the axilla (up to 50%).
A newer surgical technique known as sentinel node biopsy (SNB) has a lower risk of developing lymphoedema (<10%). The sentinel node/s are the lymph nodes that fluid from the breast ‘drains’ to first. It is thought that if cancer cells were to move from the breast they would spread to these ‘sentinel nodes’ first. SNB is a technique that aims to identify and remove just the sentinel node/s and no others. Removing only the sentinel nodes can lessen the likelihood of complications including lymphoedema.
What is the lymphatic system?
The lymphatic system is a network of tiny channels called lymph vessels. These vessels carry fluid around the body, like blood vessels carry blood around the body.
The lymph vessels carry fluid to groups of lymph nodes in the armpit, groin, neck and several other areas in the body. Lymph fluid is moved through these channels when muscles are moved when you are active.
There are particular pathways that fluid normally travels along to reach the lymph nodes. If one set of lymph nodes have been removed, the fluid is usually simply re-routed along different channels to another group of lymph nodes, because the system is able to adapt to change. However, sometimes fluid build up occurs, resulting in lymphoedema.
The lymphatic system acts to fight infection, control the immune system and help remove some of the body’s waste products. Antibodies to fight infection are made by the lymphatic system and some waste products are broken down in the lymph nodes.
What are the symptoms of lymphoedema?
People with lymphoedema usually have one or more of the following symptoms:
- Swelling of all or part of the arm.
- Swelling of the hand and fingers.
- Swelling of the breast/chest or armpit region.
- Feelings of heaviness, pain, aching, tightness or ‘bursting’ in the arm or hand.
- Skin changes such as the skin feeling thicker, harder or the skin being drier and more sensitive to irritation.
- Difficulty putting clothes or jewellery on e.g. sleeves feeling tight, rings or watches becoming tight when worn.
The early symptoms of lymphoedema may come and go, depending on things like how active you are and how hot it is.
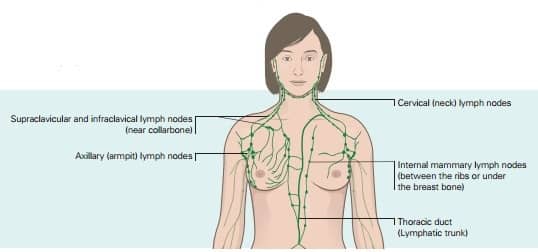
Fig 1. Lymphatic channels drain fluid from the body and carry it to the lymph nodes. The breast lymphatics drain fluid (and sometimes cancer cells) from the breast to the lymph nodes in the axilla (armpit), internal mammary chain, supraclavicular and infraclavicular areas. The sentinel lymph nodes (first lymph nodes draining a breast cancer) are found in these areas.
When is swelling not lymphoedema?
Swelling in the first few months after surgery for breast cancer is not lymphoedema. Swelling in this early stage is part of the normal process of recovering from surgery and is known as post-surgical swelling.
Any type of swelling that does not go away should be discussed with your doctor. You may need to be referred to a lymphoedema therapist. A qualified lymphoedema therapist can be found on the National Lymphoedema Practitioners Register at www.nlpr.asn.au.
Early detection helps
Early education and ongoing monitoring of any arm symptoms may reduce the onset of any long term problems of lymphoedema.
Bioimpedance Spectroscopy is a technique that measures fluid in the arm. By taking measurements before surgery and at regular intervals after surgery, lymphoedema can be detected in its early stages and treatment can be commenced even before any visible swelling is present. The L-Dex reading should be between -10 and +10 to be in the normal healthy range.
You can contact a lymphoedema therapist to have your fluid levels measured.
Caring for your arm and skin
This section gives you information on how to look after your arm and skin. Caring for your arm and skin during and after breast cancer treatment may help to lessen the risk of lymphoedema. Being aware of the things that put an added strain on the lymphatic system and reducing the levels of the amount of this activity is an important part of managing lymphoedema. Some simple guidelines on how to look after your arm are explained below.
These guidelines are also useful for women who are living with lymphoedema.
All persons who have treatment for breast cancer that includes surgery or radiotherapy to the lymph nodes should follow these guidelines.
To help prevent and manage lymphoedema it is recommended that you:
- Use the arm as normally as possible.
- Keep the skin of your arm and hand healthy and unbroken.
- Avoid using the arm in a way that puts an extra load on your lymphatic system.
All of these suggestions apply only to your arm at risk of or affected by lymphoedema. The lymphatic system in the other arm and in the rest of your body should be working normally and need no special treatment.
1. Use your arm as normally as possible
Using your arm normally helps to keep the lymph fluid moving and achieve your full range of movement quickly.
Many persons who have had treatment for breast cancer are worried that using their arm will increase their risk of developing lymphoedema. You should be able to do all of the things you were doing before you had breast cancer treatment. It is important, however, for you to be aware of your body’s signs and symptoms.
Work towards doing your normal activities:
- Start slowly, gradually building up your level of activity, rather than trying to do your previous best immediately.
- Take notice of your symptoms; your body will tell you how much you can do.
- You can do any exercises or activities including resistive training exercises such as going to a gym and doing weights training, walking, cycling, aerobics and aqua therapy and monitor for any changes or symptoms.
2. Keep the skin of your arm and hand healthy and unbroken
The skin is an important barrier against infection. If the skin is broken, bacteria can enter the body and cause infection.
An infection or repetitive infections in the arm at risk of lymphoedema (your ‘at-risk’ arm, breast and/or chest region) may cause or worsen lymphoedema in that arm. To keep your skin healthy and prevent infections, follow these simple instructions:
Keep your skin well moisturised
- Use a moisturiser every day.
- When you put moisturiser on, always stroke your arm upwards as this encourages fluid to move up your arm and away from your hand.
- Choose a simple moisturiser that does not contain perfume, as perfume can irritate the skin. Sorbolene and vitamin E cream are good choices.
- Massage around the scar using rose hip oil or a similar product twice daily for the duration of treatment and then daily thereafter for two years. Please liaise with your surgeon for further details of products you can use post surgery.
- Spend some extra time caring for the skin around your nails, as this is a place where bacteria can enter and cause infection.
- Avoid using soap on your at-risk arm as soap can dry out the skin; non-soap cleansers are better alternatives. If unsure ask your local chemist or pharmacy for soap free options.
Avoid damage to the skin of your arm and hand
- Even minor injuries to the skin such as scratches, insect bites, cuts, sunburn and places where you have had injections can be enough to cause infection in your at-risk arm.
- Consider ways that you can protect your skin. For example, wear gloves and a long-sleeved top while gardening, use an insect repellent or sunscreen, and ask health professionals to take blood pressure readings and give injections in your other arm.
- As a last resort, your treated arm can be used for injections as long as special precautions are taken by the doctor or nurse to avoid infection.
- Think about different ways you can do things to avoid injuries / infections to your skin.
If the skin of your at-risk arm gets broken, treat it quickly
- Gently wash the area with clean water.
- Use an antiseptic product to clean the wound.
- Cover the wound with a non-stick dressing.
- Avoid sticky dressings that can damage the area further when they are removed.
- Check the wound regularly over the next few days.
- See your doctor if the wound does not heal as quickly as another part of your body would, or if it looks red feels hot, or looks infected. You may need dressings or antibiotics.
3. Avoid using your arm in a way that puts an extra load on your lymphatic system
If there is extra strain on your lymphatic system for a long time, you may increase the risk of developing lymphoedema. There are several things you can do to reduce the strain on your lymphatic system.
Avoid letting your body become too hot
When the body gets hot, blood vessels open up in the skin to cool the body. This leads to an increase in the amount of fluid flowing through the skin into the lymphatic system, which may cause the arm to swell more.
Things you can do to avoid getting too hot:
- When you exercise, do so in the early morning or in the evening as these are the coolest times of the day.
- Make use of air conditioning when possible during the hot summer months.
- Pace yourself when you are doing something active. If you start to get hot, have a short break and cool down before you continue.
- Avoid putting your hand directly into hot water (greater than 34°C). This may mean wearing rubber gloves to do the washing up, using a dishwasher, or using cooler water to wash the dishes.
- Avoid getting sunburnt. Wear SPF-rated clothing and use sunscreen. Even minor burns lead to an increase in the amount of lymphatic fluid that the system has to deal with.
Try not to repeat the same movements especially if they are strenuous and cause symptoms
Some people find that if they do something with their arm over and over again (such as kneading dough, or vacuuming) their arm aches or starts to swell.
To avoid repetitive or strenuous movements pace yourself, doing intense activities in short bursts and resting, or alternating intense work with less strenuous activities. This is often more effective than trying to finish an intense activity in one go.
Avoid long periods of not moving
If you don’t move your arm muscles for a long time, lymph fluid can build up in your arm.
To avoid long periods of not moving:
- Take regular breaks to stretch and move around when you travel a long distance, (for example by bus or car).
- Use your arm as normally as possible, within the limits explained above.
- If you travel by plane, your lymphatic system is affected by both the inactivity and the change in cabin pressure. If you are planning to fly, speak to your lymphoedema therapist about things you can do to help your arm while flying. This can include wearing a compression sleeve and completing regular exercises.
Avoid activities and clothes that make your arm feel tight
Anything that is tight around your arm may block the flow of lymph fluid. This may cause swelling, even if the pressure is only there for a short period of time.
To avoid making your arm feel tight:
- When you have your blood pressure taken, ask the doctor or nurse to use your other arm.
- Avoid wearing clothing or jewellery that feels tight and cuts into your arm.
- Wear a properly fitted bra that does not leave marks in your skin.
Diet and body weight
There is no special diet that you should follow to reduce your risk of developing lymphoedema or the amount of swelling in your arm. However, eating a healthy balanced diet is advisable to maintain a healthy body weight.
Being overweight may increase the risk of lymphoedema after your breast cancer treatment. It is thought that additional fat in the arm reduces the efficiency of the lymphatic system and muscles in draining fluid.
What if I have lymphoedema?
This section explains the treatments available for lymphoedema. Following the guidelines in the previous (green) pages is also an important part of lymphoedema management.
Can lymphoedema be cured?
Early detection is the key to success! If you are aware of the symptoms of lymphoedema and seek advice early, the impact of lymphoedema on your life may be reduced. Moderate lymphoedema cannot be cured but the swelling and symptoms can be reduced and managed well by following a few simple guidelines.
How is lymphoedema treated?
If you think you may have lymphoedema, speak to your doctor for a referral to a qualified lymphoedema therapist.
A lymphoedema therapist is an occupational therapist can be an occupational therapist, physiotherapist, massage therapist, exercise physiologist, nurse or osteopath that has completed speciality training in Lymphoedema. They can be found on: www.nlpr.asn.au.
The therapist will discuss your symptoms with you and examine and measure your arm and breast/chest to find out how severe your lymphoedema is. A treatment plan can be designed for your individual situation.
Complex Lymphatic Therapy (CLT) is the usual technique used for treating lymphoedema. The aim of this treatment is to reduce the swelling and other symptoms associated with lymphoedema, and so reduce the impact of lymphoedema on your life.
This therapy program comprises:
- Draining the lymph fluid by massage (manual lymphatic drainage and self massage)
- Applying pressure (compression)
- Exercise
- Skin and arm care
- Psychological support
- Other treatments can include low level laser, use of a sequential intermittent pneumatic compression pump and compression garments.
1. Manual lymphatic drainage
This is a special form of massage that helps drain the lymph fluid, and may also help develop new pathways for lymph fluid to move around the areas that are blocked.
Manual lymph drainage uses long, slow, gentle strokes starting on the chest and stomach area, and then moving to the arm and hand. The aim is to first make a ‘space’ ready to take the extra fluid from the arm, then to move this extra fluid out of the arm.
The fluid is always moved towards the lymph nodes that are working properly; these are usually the lymph nodes in the opposite armpit and in the groin.
If your lymphoedema is severe, you may need to have manual lymph drainage performed by a therapist as part of an intensive treatment program. If the lymphoedema is less severe, you may be able to perform this massage yourself.
If there is another person who can help, the massage can also move lymph fluid across your back where there is usually no scarring from the surgery. A lymphoedema therapist can teach your partner, or a friend to perform this special massage.
2. Applying pressure (compression)
Compression has two purposes:
- It stops your arm and hand from swelling any further by providing a barrier to the swelling; and
- It helps to move the lymph fluid out of your arm and hand by helping your muscles tighten and relax.
Compression for lymphoedema can be provided by special bandages or by specially manufactured compression garments for your arm and hand.
The compression provided by garments and by bandages varies in strength. This means that the pressure is firmest at the wrist, gradually becoming less firm as it goes up the arm. This helps move the fluid out of the arm. A glove or mitten is often also used to avoid the fluid moving down to the hand and fingers instead.
Over time, both bandages and compression garments lose their stretch. It is recommended that garments be replaced after about six months of wearing them constantly. Private health funds may provide assistance to pay for garments.
3. Exercise
The lymphatic system of the arm relies on arm movements. Fluid is moved along the vessels as muscles are tightened and relaxed. Using your arm as normally as possible is an important way to try to keep the lymph fluid moving. A balance needs to be found however, because doing too much (or over-exercising) can make your symptoms worse.
There are exercise programs that help move extra fluid out of the affected arm. The exercises encourage fluid to clear first from the trunk and abdomen. Then they target the shoulder, arm and hand, to encourage the fluid to move out of the arm, and into the cleared trunk area. The exercises are gentle, and they are done each day. A lymphoedema therapist can teach you these exercises.
Resistive training exercises have also been shown to assist lymph drainage and should be encouraged.
4. Skin and arm care
You should look after your arm and skin in the same way when you have lymphoedema as you would when trying to reduce your risk of developing lymphoedema.
You should try to keep the skin healthy, prevent infection, and avoid doing things that put extra strain on your lymphatic system. See the green section ‘How to look after your arm and skin’ in this brochure.
Diet and body weight
Maintaining your weight within your ideal body weight is recommended in the management of lymphoedema. Research studies also show that even small amounts of weight loss may be helpful in reducing arm swelling.
If you have lympoedema, it is important to ensure you eat adequate protein each day as this helps to prevent your body’s muscle being broken down which may make fluid build-up worse.
There is not a lot of research conducted regarding whether a high salt diet worsens lymphoedema. However, limiting salt intake may be helpful for some people and is a general part of a healthy diet.
It is also important to ensure you drink adequate fluid each day. Reducing your fluid intake will not help reduce lymphoedema and may actually worsen it. Try to drink eight glasses of fluid each day to meet your requirements.
Things to remember about lymphoedema
- Most people who have treatment to their lymph nodes for breast cancer do not get lymphoedema.
- The lymphatic system adapts very well, and after treatment for breast cancer, other lymph nodes are usually able to take over the work that was done by the lymph nodes in the armpit.
- Use your arm as normally as possible. Be aware of possible symptoms, and adjust what you do accordingly.
- Do not do things that consistently cause your symptoms to appear. If doing a certain thing seems to cause symptoms such as arm swelling, you should rest, and elevate your arm. Swelling that lasts for only a short time and settles with simple measures such as raising your arm up may mean that your lymphatic system is under strain.
- If you are able to do an activity without noticing any symptoms, it is safe to continue doing this activity without concern.
- If you develop symptoms that do not go away or you are worried about developing lymphoedema, talk to your doctor who may refer you to a lymphoedema clinic to be assessed by a lymphoedema therapist.
- Remember that early detection is important and early symptoms of lymphoedema can be managed well. Discuss your symptoms with your doctor, or lymphoedema therapist
Contacts
Westmead Breast Cancer Institute
Westmead Hospital
(02) 8890 8888
Lymphoedema Clinic
Westmead Hospital
(02) 8890 6500
Lymphoedema Support Group NSW
https://www.lymphoedemasupport.com/
Choose a qualified Lymphoedema Therapist with confidence.
National Lymphoedema Practitioners Register
A service of the Australasian Lymphology Association
A public register of lymphoedema practitioners in Australia and New Zealand. These practitioners fulfil the accreditation and registration requirements of the Australasian Lymphology Association
Dietitians Association of Australia (DAA)
Accredited Practising Dietitians are registered nutrition professionals who are able to offer personalised advice about maintaining a healthy diet and achieving a healthy weight.
Useful contacts/websites
| Cancer Australia | canceraustralia.gov.au |
| Cancer Council | cancer.org.au |
| Cancer Council Helpline | 13 11 20 |
| Breast Cancer Network Australia (BCNA) | 1800 500 258 bcna.org.au |
[This information guide is also available in PDF format to download.]
Version 5 – WSP 115 February 2024
© Westmead Breast Cancer Institute
