[This information guide is also available in PDF format to download.]
Hormonal (endocrine) therapies for breast cancer (also called ‘anti-hormone treatment’)
Hormonal therapy is used to treat breast cancers that are hormone receptor positive. These cancers have receptors for the hormones oestrogen and/or progesterone; they are called ER and/or PR positive cancer. Around 70% of breast cancers are ER positive.
Hormonal therapy may be recommended after other treatments for breast cancer like surgery, chemotherapy or radiotherapy. Sometimes it is used to shrink breast cancer before other treatment is given. The aim of hormonal therapy is to ‘starve’ breast cancer cells of the hormone (oestrogen) that makes them grow. This lowers the risk of breast cancer coming back or a new breast cancer developing in the treated breast or in the other breast.
There are several different types of hormonal therapies. Some are taken as tablets (tamoxifen or aromatase inhibitors) and others may involve surgery, injections or radiotherapy to turn off ovaries in premenopausal women.
This brochure explains the following types of hormonal therapies to turn off ovaries in premenopausal women:
- tamoxifen
- aromatase inhibitors
- ‘turning off’ or removing the ovaries
Hormonal therapies can also be used to treat ductal carcinoma in situ (DCIS) and to reduce the risk of breast cancer in women with a strong family history or other risk factors for breast cancer.

What are hormone receptors?
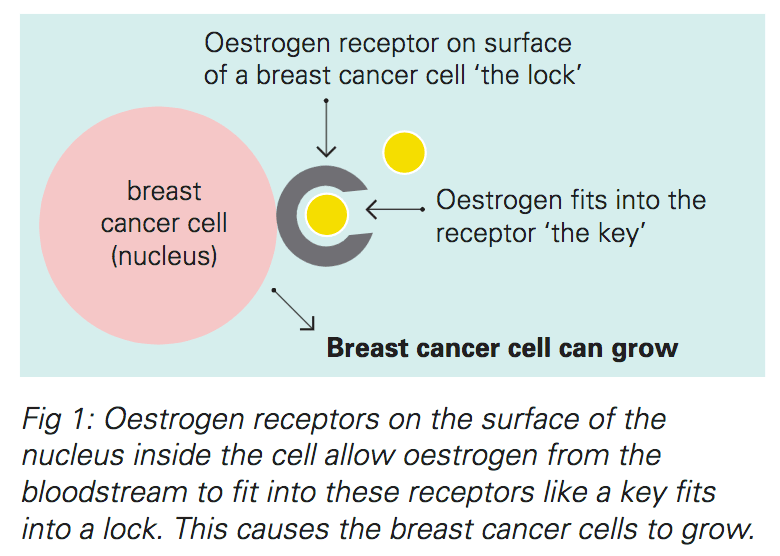
Breast cancers that are hormone receptor positive have receptors for the female hormones oestrogen and/or progesterone on the inside of the cancer cells.
In breast cancer cells that are hormone receptor positive, oestrogen and/or progesterone, which are naturally produced in the body, make the cancer grow. You can think of it as the receptor being the lock and oestrogen being the key. The oestrogen fits into the receptor and switches the cancer cell on, causing it to grow. Hormone therapy for breast cancer can ‘starve’ cancer cells by upsetting this process.
Testing for hormone receptors is part of the routine pathology testing following surgery. Testing is done on a core biopsy sample if surgery is not planned. Your doctor will be able to tell you if your breast cancer is hormone receptor positive or not. Most breast cancer (around 70%) is hormone receptor positive.
The hormonal therapies described in this brochure only work against breast cancers that are hormone receptor positive. Other treatments need to be used for cancers that are hormone receptor negative.
Tamoxifen
Tamoxifen has been used for many years to treat breast cancer. It has been proven to be a very effective treatment. Tamoxifen can substantially reduce the chance of breast cancer coming back and of new breast cancers developing.
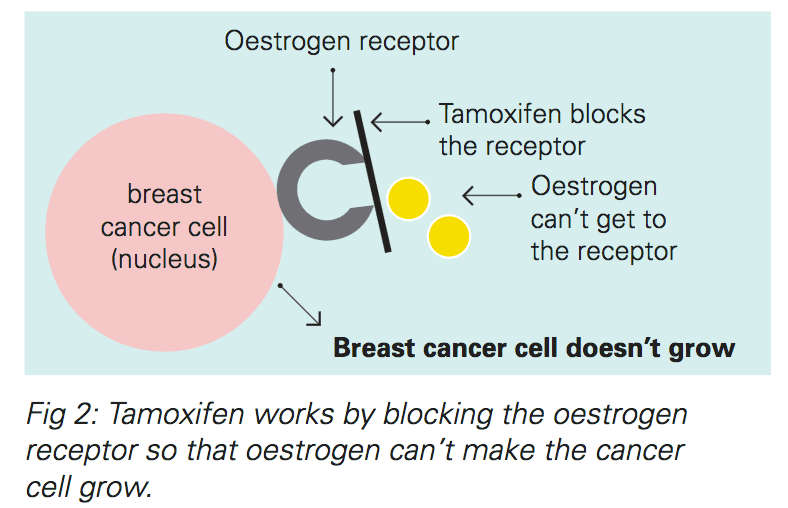
Tamoxifen works by blocking the oestrogen receptor inside the breast cancer cell. This stops oestrogen making the breast cancer cell grow.
Tamoxifen is taken as a tablet once a day. It may be prescribed as a five-year course after other treatments for early breast cancer like surgery, chemotherapy and radiotherapy have been completed. In some cases tamoxifen is prescribed for two or three years before switching to a different hormonal therapy like an aromatase inhibitor (see next section). Sometimes tamoxifen is recommended for up to ten years. If tamoxifen is being used to treat metastatic breast cancer (breast cancer that has spread beyond the breast), it is used for as long as it keeps working.
Tamoxifen is a very effective hormonal therapy for women before or after menopause.
Tamoxifen:
- reduces the risk of early breast cancer coming back
- reduces the risk of new breast cancer developing
- can be used after other treatments for breast cancer like radiotherapy and chemotherapy
- strengthens bones rather than reducing bone density unlike aromatase inhibitors
- may lower cholesterol and reduce the risk of developing heart disease
- works either before or after menopause
Side effects
Most women do not experience significant side effects while taking tamoxifen.
Tamoxifen does not cause menopause, but its side effects are like those that many women experience after menopause
Common side effects:
- hot flushes and sweats
- irregular vaginal bleeding in women who have not been through menopause
- vaginal irritation, dryness or discharge
- fluid retention and weight gain
Uncommon side effects:
- light-headedness, dizziness, headache
- tiredness
- rash
- nausea
- depression or mood swings
Rare side effects:
-
Blood clots in the veins in the legs (deep venous thrombosis, DVT) or lungs (pulmonary embolus). The risk of clots while taking tamoxifen is about the same as the risk of blood clots for women who take the oral contraceptive pill or hormone replacement therapy. Clots are more common in women who have a family history of blood clots or have an inherited risk of blood clots. Before starting tamoxifen, tell your doctor if you have ever had a blood clot.
-
Cancer of the endometrium (lining of the uterus) may develop in less than 1% of women taking tamoxifen for more than 10 years. It is important that you report any abnormal vaginal bleeding to your cancer specialist (oncologist) because sometimes more tests are needed.
-
eye problems—tell your doctor if you notice any change in your vision
Very rare side effects:
- hair thinning
- changes in blood tests (liver function)
- changes in memory and thinking
If you are worried about side effects, talk to your doctor
Fertility issues
You should not become pregnant or breast feed while taking tamoxifen or for 1–2 months after stopping tamoxifen.
Tamoxifen can increase fertility so you must use contraception while you are taking tamoxifen if you have not been through menopause. Use a barrier method such as condoms, a diaphragm or a non-hormonal intra-uterine device (IUD). You must not take the oral contraceptive pill with tamoxifen.
Taking other medications with tamoxifen
Tamoxifen can interact with Warfarin (a drug used to thin the blood to prevent blood clotting). If you take Warfarin you should tell your doctor.
You should not take other hormone medications while you take tamoxifen. You can continue to take all other medications prescribed by your doctor.
Aromatase inhibitors
Aromatase inhibitors are another hormone treatment for breast cancer. They are an alternative to tamoxifen. Aromatase inhibitors only work in post-menopausal women. Women who are post-menopausal, either naturally or as a result of treatment such as chemotherapy or surgical removal of the ovaries, may be prescribed aromatase inhibitors.
If you and your doctor don’t know whether or not you have gone through menopause, you may be prescribed tamoxifen for a year or more and then changed to an aromatase inhibitor once menopause is confirmed. If you have not been through menopause these drugs do not work effectively.
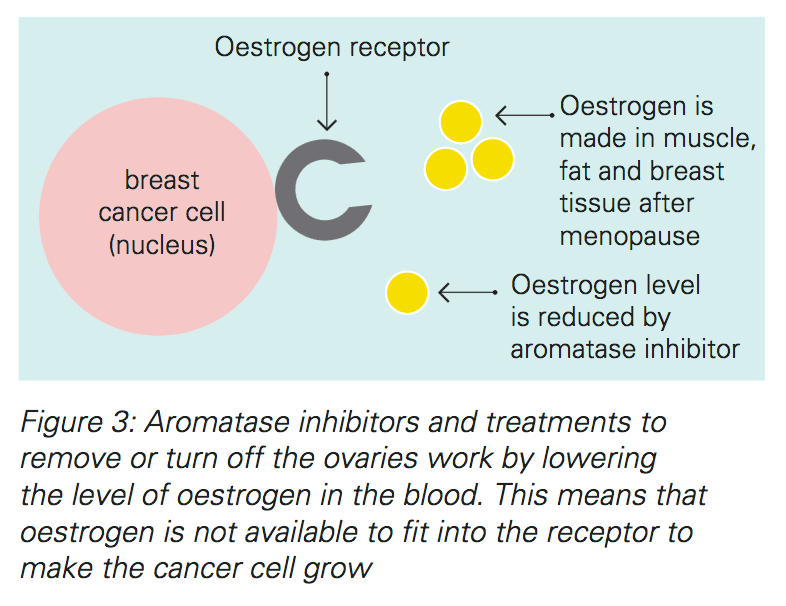
In women before menopause, most if not all oestrogen is made in the ovaries. After menopause, an enzyme called aromatase helps to make oestrogen in the peripheral body tissues such as muscle, fat and the adrenal glands. Aromatase inhibitors work by blocking this enzyme, thereby reducing the production of oestrogen to feed the breast cancer cells.
Aromatase inhibitors are taken as a tablet once a day. The treatment course is usually five years.
Like tamoxifen, aromatase inhibitors can be used before or after other treatments for breast cancer such as surgery, chemotherapy and radiotherapy.
Aromatase inhibitors can also be used after two to three years of tamoxifen to complete the course of hormonal treatment. Sometimes, a 10-year course of aromatase inhibitor is recommended. Aromatase inhibitors can also be used to treat breast cancer that has recurred or spread.
Three aromatase inhibitors are used in Australia:
- anastrazole (Arimidex®)
- letrozole (Femara®)
- exemestane (Aromasin®)
Aromatase inhibitors:
- reduce the risk of early breast cancer coming back in the future
- reduce the risk of new breast cancer developing
- can be used with other treatments like radiotherapy and chemotherapy
- are slightly more effective than tamoxifen
- does not cause blood clots or cancer of endometrium (the lining of the uterus)
Side effects
Common side effects:
- aches and pain of muscles and joints
- hot flushes
- vaginal dryness
Uncommon side effects:
- reduced sex drive
- osteoporosis or thinning of bone
- insomnia
- fatigue
Looking after your bones while taking an aromatase inhibitor
Aromatase inhibitors can reduce bone density. This may increase the risk of bone fracture.
To keep your bones healthy while you are taking this medication, your doctor may recommend that you:
- have a bone density test before and during treatment
- do regular weight-bearing exercise
- maintain a healthy intake of calcium
- ensure a healthy intake of vitamin D
- take other prescription medications to build up your bones if your bone density is already low
If you do show signs of bone thinning (osteopenia) or weakening (osteoporosis) you may need to see your GP or specialist for special treatment for your bones.

‘Turning off’ or removing the ovaries ‘
‘Turning off’ or removing the ovaries lowers the levels of oestrogen in the blood. This is another way of ‘starving’ cancer cells of oestrogen to stop them growing. This treatment only works before menopause. This treatment is not necessary for women who have already gone through menopause because the ovaries naturally stop making oestrogen after menopause.
Turning off or removing the ovaries:
- reduces the risk of cancer returning or new cancer developing
- can be combined with other treatments for breast cancer like breast surgery, radiotherapy, chemotherapy, aromatase inhibitors and tamoxifen
Surgical removal of the ovaries reduces the risk of breast cancer returning and has the added benefit of reducing the risk of developing cancer of the ovaries, although cancer of the ovaries is uncommon.
Turning off the ovaries with medication
The ovaries can be shut down temporarily with medication. This is usually done by giving monthly injections of goserelin (Zoladex®). This gradually causes the levels of oestrogen to fall, which leads to temporary menopause.
The menstrual periods stop and other symptoms of menopause may develop (see below). These symptoms can be reversed. If the injections are stopped, the oestrogen levels and menstrual periods return to normal.
Some women who are considering having their ovaries removed have these injections for a few months to ‘test out’ the menopausal symptoms. They still have the choice of reversing the effect if the side effects are too intense.
Side effects
-
Symptoms of menopause: hot flushes, mood swings, difficulty sleeping, vaginal dryness.
-
These symptoms usually come on gradually over weeks or months as the levels of oestrogen drop slowly.

Surgical removal of the ovaries
The operation to remove the ovaries is called oophorectomy. Surgical removal of the ovaries is a permanent way to reduce the levels of oestrogen. It is a very effective treatment to stop early breast cancer returning or to slow the progress of metastatic cancer. This can also reduce the risk of developing ovarian cancer.
Surgery to remove the ovaries can be done with keyhole surgery (using a laparoscope) or with an open operation (making an incision along the bikini line). Your surgeon will discuss with you the pros and cons of these different techniques. Oophorectomy is done under a general anaesthetic (while you are asleep). Usually the fallopian tubes are also removed but the uterus (womb) is left intact.
After oophorectomy, the symptoms of menopause may come on suddenly. This is different to turning off the ovaries with medication which brings menopausal symptoms on gradually.
Side effects
-
Symptoms of menopause: hot flushes, mood swings, difficulty sleeping, vaginal dryness. These may start suddenly in the few days following the operation.
-
Side effects of the surgical procedure itself are possible. These vary depending on how the procedure is done. Your surgeon will discuss these with you in more detail
-
Side effects of the anaesthetic are possible.
If you do get troublesome side-effects on these treatments, we can often find a different drug or a different dose that will help, so it is important not to just stop the drug, but to talk to your specialist.
Menopausal symptoms
All of the hormonal therapies described in this brochure reduce the effects of oestrogen in your body.This means that they can all cause symptoms of menopause like hot flushes, mood swings, vaginal symptoms and a change in sex drive.
The range and severity of menopausal symptoms vary from one woman to another. Some women may experience very few menopausal symptoms. Symptoms will usually become less noticeable with time, as the body adjusts to lower oestrogen levels.
In general, hormone replacement therapy is not recommended in women who have had breast cancer but there are other things that can help. More information can be found in the ‘Menopause’ brochure.
Who can I speak to?
If you would like more information about hormone treatment ask your surgeon, cancer specialist (oncologist), breast care nurse or other health professional.
Useful contacts/websites
| Cancer Australia | canceraustralia.gov.au |
| Cancer Council | cancer.org.au |
| Cancer Council Helpline | 13 11 20 |
| Breast Cancer Network Australia (BCNA) | 1800 500 258 bcna.org.au |
Version 7 – WSP 232 February 2024
© Westmead Breast Cancer Institute
[This information guide is also available in PDF format to download.]
