[This information guide is also available in PDF for download.]
Caring for your breasts
Breast cancer is common and will affect 1 in 8 Australian women by the age of 85. It is more common among older women. Almost three-quarters of breast cancers develop in women over the age of 50. The earlier breast cancer is found, the simpler the treatment and the better the outcome.
Checking your breasts
If you are aware of how your breasts usually look and feel you are more likely to notice a change if it develops. You should check your breasts regularly, so that you are familiar with their usual look and feel. Most women find that their breasts are easier to examine just after their period when any premenstrual lumpiness and pain has settled. If you don’t get periods, you can check your breasts at any time. It is recommended that you check your breasts at least every few months.
You can check your breasts by:
- looking at the shape and appearance of the breasts and nipples in the mirror with your hands by your sides
- raising your arms above your head and looking for a change in the shape of the breasts
- feeling for lumps in the breasts either while lying down or standing (for example, in the shower)
- feeling for lumps in the nipple area and in the armpits.
A simple way to check your breasts is explained in this brochure. Your doctor can also show you how to check your breasts.
How to check your breasts
Checking your breasts is simple. You may feel awkward doing this the first time but it gets easier as you get used to it. To check your breasts you need to look at your breasts in the mirror and then feel your breast for lumps.
When you check your breasts in the mirror, look for:
- changes in the size and shape
- dimpling, puckering or skin changes
- anything different about your nipples.
Checking your breasts
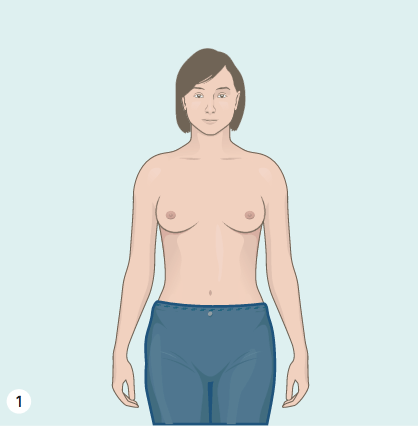
Step 1
Step 1
Undress from the waist up and stand in front of the mirror. Look in the mirror with your arms by your side. Notice the shape. Look for dimpling (a ‘dent’ in the smooth contour of the breasts) and nipple changes (such as a rash or ‘pulled in’ appearance). Look for differences between the two breasts.
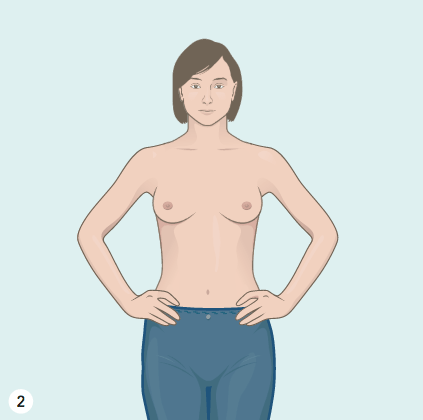
Step 2
Step 2
Look at your breasts in the mirror with your hands on your hips and your chest muscles tightened. Again, look for changes in the breast shape, the nipple appearance or differences between the breasts.
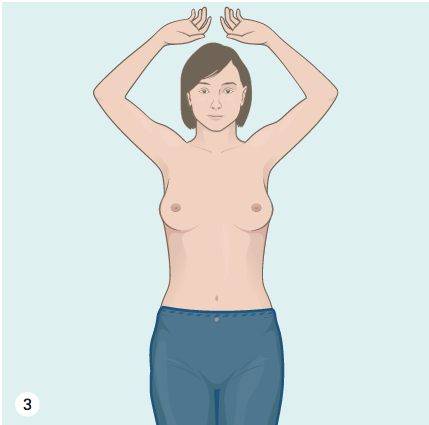
Step 3
Step 3
Look at your breasts with your arms raised high above your head. The breasts should move up slightly and equally when the arms are raised. Areas of dimpling may be more obvious in this position.
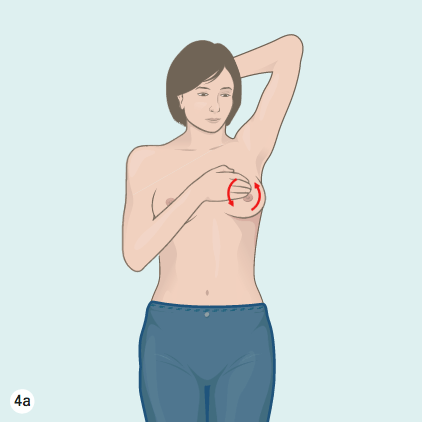
Step 4a
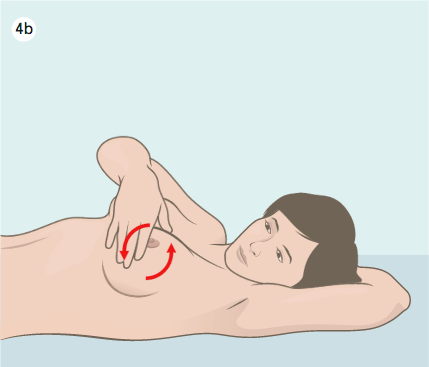
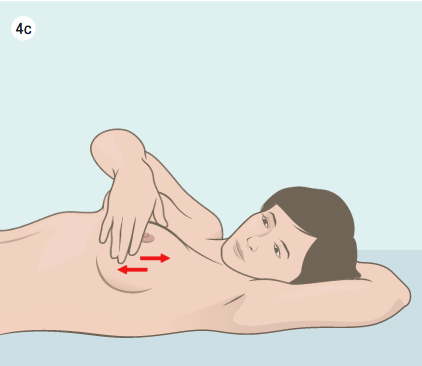
Step 4b
Step 4c
Step 4
Next, feel your breasts for lumps. This can be done while standing (4a) or lying (4b and 4c).
Use your flattened fingers to feel each part of the breast. This can be done in circles (4a and 4b), in strips up and down the breast (4c) or by examining each quadrant (quarter) of the breast in turn.
The most important thing is to make sure that you feel the whole breast, from your collarbone to the bottom of your lowest ribs and from your armpit to the centre of your chest. It is also important to feel underneath the nipple (but don’t squeeze the nipple).
Sometimes breast lumps are very obvious and they feel like a firm pea or grape. Other times lumps just feel like a thickened area that stands out a little from the surrounding tissue. If you find something that is new or is different to the other breast, you should talk to your doctor about it.
Remember, most breast changes are not caused by cancer but they should always be checked just to be sure.
Breast changes
Changes in the breasts may be warning signs of breast cancer. All of these changes can also have benign (non-cancerous) causes. These benign causes are more common than cancerous causes. However, if you notice any of these changes, you should have your breasts checked by a doctor.
The changes to look for include:
- a lump or lumpiness
- any change in the shape or appearance of the breast such as dimpling or redness
- an area that feels different to the rest of the breast
- any change in the shape or appearance of the nipple, such as the nipple being pulled in or developing a rash
- a discharge from the nipple, especially if it is bloody or it happens without squeezing the nipple
- pain in the breast that is unusual for you.
What if I find a change?
If you think there may be a change in the way your breasts look or feel, don’t panic. While it is important to have it checked, most breast changes are not related to cancer. It is safe to watch the area for a couple of weeks to see if it improves. Some breast changes will settle down after your menstrual period. If you think the area is still different after your next period, see your doctor for a breast examination. Your doctor may order some tests.
You should discuss breast changes with your doctor rather than arranging a free screening mammogram yourself because you may need more than just a mammogram.
Clinical breast examination
Clinical breast examination (CBE) is a breast examination done by a doctor or nurse qualified in CBE. As well as checking your own breasts, it is a good idea to see your doctor or qualified nurse every 1-2 years for a breast examination. Sometimes they will notice changes that you have not noticed.
Screening mammograms
A mammogram is an X-ray of the breast. It is recommended that every woman over the age of 50 has a mammogram every two years. Some women worry that a mammogram will be painful. Squeezing the breast (compression) during a mammogram is important to get good pictures of the breast. This can be uncomfortable but it only lasts for a short time. If you are experiencing pain or discomfort, talk to the person performing your mammogram who will be able to assist you.
A mammogram is the best test for picking up breast cancer at a very early stage. Mammograms are free for all women aged 50–74 through the BreastScreen program. Woman aged between 40 and 49 and women over 74 can also have free mammograms through this program, on request.
Mammograms pick up around 90% of breast cancers. This means that there are some breast cancers that will not be seen on a mammogram. Therefore, it is important that if you have a breast symptom you have this checked by your doctor because you may need other tests like an ultrasound or biopsy.
There are some women who should have mammograms every year rather than every two years. This includes women who have a family history of breast cancer in several close relatives and women who have had breast cancer.
Screening mammograms are not generally recommended for women under 40. These younger women should check their own breasts for changes and see their doctor or nurse qualified in CBE every year for a clinical breast examination.
Family history and breast cancer
Most breast cancer develops in women who do not have a family history of breast cancer. Women who have several close relatives who have had breast cancer or ovarian cancer may be at a higher-than-average risk. Some families carry a gene fault that increases the chances of breast cancer developing.
If you are worried about your family history of breast or ovarian cancer, discuss this with your doctor who may recommend a referral to a family cancer clinic.
Family cancer clinics can give you specific advice about your individual risk and can arrange testing for gene faults in the family if this is needed.
More information can be found in the brochure Family history of breast cancer.
Hormone replacement therapy (HRT)
Using hormone replacement therapy (HRT) may cause a small increase in the risk of developing breast cancer.
While there has been a lot of worry about HRT in the past, more recent research has shown that the risk may not be as high as once thought. The risk seems to be highest in those who use HRT for more than five years. The best advice is to avoid HRT if possible, but if it is needed to control hot flushes or other side-effects of menopause, it should be used for no longer than five years.
Contact numbers
Westmead Breast Cancer Institute 8890 6728
BreastScreen NSW 13 20 50
Useful contacts/websites
| Cancer Australia | canceraustralia.gov.au |
| Cancer Council | cancer.org.au |
| Cancer Council Helpline | 13 11 20 |
| Breast Cancer Network Australia (BCNA) | 1800 500 258 bcna.org.au |
[This information guide is also available in PDF for download.]
Version 5 – WSP 202 February 2022
© Westmead Breast Cancer Institute
